This information was published by Bupa's health information team and is based on reputable sources of medical evidence. It has been peer reviewed by Bupa doctors. The content is intended for general information only and does not replace the need for personal advice from a qualified health professional.
Key points
● Pharyngitis most commonly occurs in school-aged children during the winter months.
● Pharyngitis is usually caused by an infection with a virus but can sometimes be caused by group A Streptococcus bacteria.
● The most common symptom of pharyngitis is a sore throat.
● Antibiotics aren’t routinely prescribed to treat a sore throat.
● Pharyngitis usually gets better without treatment within three to seven days.
Key points
● Pharyngitis most commonly occurs in school-aged children during the winter months.
● Pharyngitis is usually caused by an infection with a virus but can sometimes be caused by group A Streptococcus bacteria.
● The most common symptom of pharyngitis is a sore throat.
● Antibiotics aren’t routinely prescribed to treat a sore throat.
● Pharyngitis usually gets better without treatment within three to seven days.
About pharyngitis
Pharyngitis is the medical term used to describe an infection or inflammation of your throat.
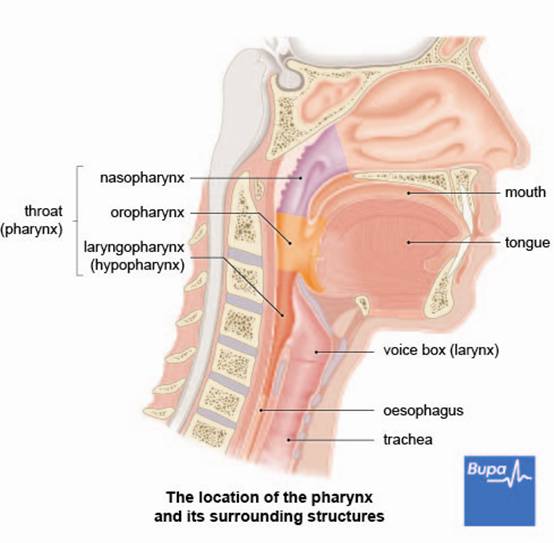
Your throat starts at the back of your mouth and nose and connects to your oesophagus (the pipe that goes from your mouth to your stomach), windpipe (trachea) and voice box (larynx).
Your throat starts at the back of your mouth and nose and connects to your oesophagus (the pipe that goes from your mouth to your stomach), windpipe (trachea) and voice box (larynx).
Pharyngitis can be an acute or chronic inflammation of your throat. When describing an illness, the terms ‘acute’ and ‘chronic’ refer to how long a person has had it, not to how serious the condition is.
- Acute pharyngitis is typically over within three to seven days. It’s a common condition, particularly in children aged five to 15 years old during winter and early spring.
- Chronic pharyngitis (or a persistent sore throat) lasts for longer, sometimes for several weeks.
Symptoms of pharyngitis
The symptoms of pharyngitis vary depending on how inflamed your throat is. The most common symptom is a sore throat, which may be mild or severe. Other symptoms that you may also have at the same time include:
- difficulty and pain when swallowing
- a fever (a temperature higher than 37.5°C)
- a runny or blocked nose
- a cough
- a headache
- enlarged and tender glands in your neck
- pain or discomfort in your abdomen (tummy)
- feeling sick or vomiting
- enlarged and painful tonsils (tonsillitis)
Complications of pharyngitis
Most people with pharyngitis won’t have any complications. However, on rare occasions, pharyngitis caused by a bacterial infection can lead to:
You’re more likely to develop complications if you have a weakened immune system, for example if you have HIV/AIDS, or are taking medicines that suppress your immune system.
- tonsillitis – see our frequently asked questions for more information of ear infection (otitis media)
- a sinus infection (sinusitis)
- a throat abscess (retropharyngeal abscess) – this is most common in young children
- an abscess behind your tonsils (peritonsillar abscess or quinsy)
You’re more likely to develop complications if you have a weakened immune system, for example if you have HIV/AIDS, or are taking medicines that suppress your immune system.
Causes of pharyngitisv
Pharyngitis is usually caused by an infection with a virus and, less commonly, by bacteria. Most people with acute pharyngitis have a viral infection such as the common cold virus. The most common type of bacterial infection is group A Streptococcus (known as strep throat). Strep throat occurs most often in children. There is no evidence that sore throats caused by a bacterial infection are more severe than those caused by a virus, or that they last any longer.
Other, rarer causes of an acute sore throat may include:
Other, rarer causes of an acute sore throat may include:
- a thrush infection of your throat
- a sexually transmitted infection passed on through oral sex
- a blood disorder, such as leukaemia or anaemia
- certain medicines such as carbimazole, clozapine and sulfasalazine
Diagnosis of pharyngitis
You probably won’t need to see your GP if you or your child has a sore throat. However, if you’re worried that your symptoms are more severe or not getting better, contact your GP – he or she may be able to advise you.
Your GP will usually be able to diagnose pharyngitis by asking about your symptoms and possibly also examining you. He or she may look inside your throat to check for signs of infection and feel your neck to check for any swelling. You won't usually need any other tests but if your GP suspects you have a bacterial infection and you’re at risk of complications, he or she may take a swab sample from the back of your throat to help confirm this. However, this isn't usually necessary.
Your GP may also ask you to have a blood test to check for glandular fever if you have a sore throat that lasts for longer than a week.
If you have had a sore throat for longer than three weeks with no obvious cause, your GP may refer you to a doctor who specialises in ear, nose and throat conditions.
Your GP will usually be able to diagnose pharyngitis by asking about your symptoms and possibly also examining you. He or she may look inside your throat to check for signs of infection and feel your neck to check for any swelling. You won't usually need any other tests but if your GP suspects you have a bacterial infection and you’re at risk of complications, he or she may take a swab sample from the back of your throat to help confirm this. However, this isn't usually necessary.
Your GP may also ask you to have a blood test to check for glandular fever if you have a sore throat that lasts for longer than a week.
If you have had a sore throat for longer than three weeks with no obvious cause, your GP may refer you to a doctor who specialises in ear, nose and throat conditions.
Treatment of pharyngitis
For most people, a sore throat will get better on its own within a week of the symptoms starting without any specific treatment. However, there are things you can do to help ease your symptoms and make you feel more comfortable.
Self-help
Although there is little scientific evidence to support it, you may find gargling a few times a day for three to four minutes with salt water or soluble aspirin dissolved in water helps your sore throat. Never give aspirin to children under the age of 16. Drinking warm liquids (particularly with lemon and honey) and sucking on throat lozenges may also help to soothe your throat.
Medicines
Over-the-counter painkillers
You can take over-the-counter painkillers such as ibuprofen or paracetamol to relieve pain and reduce your temperature. Don’t give aspirin to children under 16. Always read the patient information leaflet that comes with your medicine and if you have any questions, ask your pharmacist for advice. If your symptoms don’t improve or get worse, contact your GP.
Antibiotics
Your GP is unlikely to prescribe antibiotics, even if your sore throat is thought to be caused by a bacterial infection, as they won't usually relieve your symptoms or help you to recover any sooner. You may be prescribed antibiotics if you have a severe infection or if your GP thinks you're at risk of complications. You may also be given antibiotics if you're admitted to hospital because of a complication, such as an abscess.
If you're prescribed antibiotics, make sure that you take the full course. Your GP will usually give you penicillin to take by mouth for 10 days. If you’re allergic to penicillin, your GP will prescribe an alternative antibiotic. Always ask your GP for advice and read the patient information leaflet that comes with your medicine.
Self-help
Although there is little scientific evidence to support it, you may find gargling a few times a day for three to four minutes with salt water or soluble aspirin dissolved in water helps your sore throat. Never give aspirin to children under the age of 16. Drinking warm liquids (particularly with lemon and honey) and sucking on throat lozenges may also help to soothe your throat.
Medicines
Over-the-counter painkillers
You can take over-the-counter painkillers such as ibuprofen or paracetamol to relieve pain and reduce your temperature. Don’t give aspirin to children under 16. Always read the patient information leaflet that comes with your medicine and if you have any questions, ask your pharmacist for advice. If your symptoms don’t improve or get worse, contact your GP.
Antibiotics
Your GP is unlikely to prescribe antibiotics, even if your sore throat is thought to be caused by a bacterial infection, as they won't usually relieve your symptoms or help you to recover any sooner. You may be prescribed antibiotics if you have a severe infection or if your GP thinks you're at risk of complications. You may also be given antibiotics if you're admitted to hospital because of a complication, such as an abscess.
If you're prescribed antibiotics, make sure that you take the full course. Your GP will usually give you penicillin to take by mouth for 10 days. If you’re allergic to penicillin, your GP will prescribe an alternative antibiotic. Always ask your GP for advice and read the patient information leaflet that comes with your medicine.
Common questions
1. What is the difference between pharyngitis and tonsillitis?
Answer
Pharyngitis is inflammation of your throat (pharynx), whereas tonsillitis is inflammation of your tonsils. A sore throat is a symptom of both pharyngitis and tonsillitis.
Explanation
Pharyngitis and tonsillitis are very similar conditions and can be hard to distinguish. A sore throat can be a symptom of either condition, so they are sometimes both referred to as an ‘acute sore throat’. The only real difference between the two conditions is the part of your throat that is affected.
The two conditions are treated in a similar way. However, if you have recurrent or chronic tonsillitis, your doctor may recommend surgery to remove your tonsils. Recurrent and chronic pharyngitis can be more difficult to treat, but understanding the causes can help to manage the condition. For example, if you drink alcohol regularly or smoke, drinking less and stopping smoking may help improve your symptoms.
2. Can I catch pharyngitis from someone who has it?
Answer
Yes, it's possible that you could catch the infection that has caused pharyngitis in another person.
Explanation
Pharyngitis is usually caused by an infection with a virus (such as the common cold) or group A Streptococcus bacteria.
You’re most likely to catch the infection that causes pharyngitis by coming into contact with an infected person, for example by shaking hands with someone who has a sore throat, or by touching something an infected person has recently touched. You pick up the virus or bacteria on your hands and then, when you touch your nose or mouth, you may pass it to yourself.
The best way to reduce your risk of infection is to regularly wash your hands and try to stay away from people who have symptoms of cold or flu. If you have cold or flu symptoms, cover your mouth when coughing or sneezing, throw used tissues in the bin and wash your hands regularly to reduce the risk of spreading the infection.
3. Why aren't antibiotics usually prescribed to treat pharyngitis?
Answer
Antibiotics aren't usually helpful in relieving the symptoms of pharyngitis, or in reducing the duration of your illness.
Explanation
Pharyngitis is most often caused by a viral infection such as the common cold. Antibiotics only work against bacteria and so aren't effective at treating viral infections.
Your GP won't usually prescribe antibiotics, even if your sore throat is thought to be caused by a bacterial infection. This is because antibiotics haven’t been found to be much more effective than painkillers in relieving your symptoms or in helping you to recover any sooner.
Taking antibiotics when they aren't necessary can increase your risk of developing antibiotic resistance – this means that the medicine isn’t effective at getting rid of the infection. Antibiotics can also cause unpleasant side-effects such as diarrhoea and a rash.
Your GP may think it necessary to prescribe antibiotics if you have a severe illness that is likely to be caused by a bacterial infection, or if he or she thinks you're at increased risk of complications.
If you're prescribed antibiotics, make sure that you take the full course. Your GP will usually give you penicillin to take by mouth for 10 days. If you’re allergic to penicillin, your GP will prescribe a different antibiotic. Always ask your GP for advice and read the patient information leaflet that comes with your medicine.
Answer
Pharyngitis is inflammation of your throat (pharynx), whereas tonsillitis is inflammation of your tonsils. A sore throat is a symptom of both pharyngitis and tonsillitis.
Explanation
Pharyngitis and tonsillitis are very similar conditions and can be hard to distinguish. A sore throat can be a symptom of either condition, so they are sometimes both referred to as an ‘acute sore throat’. The only real difference between the two conditions is the part of your throat that is affected.
- Pharyngitis means inflammation of your pharynx. This is the part of your throat that starts at the back of your mouth and nose and connects them to your oesophagus (the pipe that runs from your mouth to your stomach), windpipe (trachea) and voice box (larynx).
- Tonsillitis is inflammation of your tonsils, which are the glands at the back of your throat.
The two conditions are treated in a similar way. However, if you have recurrent or chronic tonsillitis, your doctor may recommend surgery to remove your tonsils. Recurrent and chronic pharyngitis can be more difficult to treat, but understanding the causes can help to manage the condition. For example, if you drink alcohol regularly or smoke, drinking less and stopping smoking may help improve your symptoms.
2. Can I catch pharyngitis from someone who has it?
Answer
Yes, it's possible that you could catch the infection that has caused pharyngitis in another person.
Explanation
Pharyngitis is usually caused by an infection with a virus (such as the common cold) or group A Streptococcus bacteria.
You’re most likely to catch the infection that causes pharyngitis by coming into contact with an infected person, for example by shaking hands with someone who has a sore throat, or by touching something an infected person has recently touched. You pick up the virus or bacteria on your hands and then, when you touch your nose or mouth, you may pass it to yourself.
The best way to reduce your risk of infection is to regularly wash your hands and try to stay away from people who have symptoms of cold or flu. If you have cold or flu symptoms, cover your mouth when coughing or sneezing, throw used tissues in the bin and wash your hands regularly to reduce the risk of spreading the infection.
3. Why aren't antibiotics usually prescribed to treat pharyngitis?
Answer
Antibiotics aren't usually helpful in relieving the symptoms of pharyngitis, or in reducing the duration of your illness.
Explanation
Pharyngitis is most often caused by a viral infection such as the common cold. Antibiotics only work against bacteria and so aren't effective at treating viral infections.
Your GP won't usually prescribe antibiotics, even if your sore throat is thought to be caused by a bacterial infection. This is because antibiotics haven’t been found to be much more effective than painkillers in relieving your symptoms or in helping you to recover any sooner.
Taking antibiotics when they aren't necessary can increase your risk of developing antibiotic resistance – this means that the medicine isn’t effective at getting rid of the infection. Antibiotics can also cause unpleasant side-effects such as diarrhoea and a rash.
Your GP may think it necessary to prescribe antibiotics if you have a severe illness that is likely to be caused by a bacterial infection, or if he or she thinks you're at increased risk of complications.
If you're prescribed antibiotics, make sure that you take the full course. Your GP will usually give you penicillin to take by mouth for 10 days. If you’re allergic to penicillin, your GP will prescribe a different antibiotic. Always ask your GP for advice and read the patient information leaflet that comes with your medicine.
Disclaimer
This information was published by Bupa Group's Health Content Team and has been reviewed by appropriate medical or clinical professionals. To the best of their knowledge the information is current and based on reputable sources of medical evidence, however Bupa (Asia) Limited makes no representation or warranty as to the completeness or accuracy of the Content.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites.
Resources
Further information
- ENT UK - 020 7404 8373 - www.entuk.org
- Acute pharyngitis. BMJ Best Practice.www.bestpractice.bmj.com, published 19 October 2012
- Sore throat – acute. NICE Clinical Knowledge Summaries. cks.nice.org.uk, published October 2012
- Viral pharyngitis. eMedicine. www.emedicine.medscape.com, published 26 September 2011
- Pediatric pharyngitis. eMedicine. www.emedicine.medscape.com, published 15 June 2012
- Management of sore throat and indications for tonsillectomy. Scottish Intercollegiate Guidelines Network (SIGN), April 2010. www.sign.ac.uk
- Vincent MT, Celestin N, Hussain AN. Pharyngitis. Am Fam Physician 2004; 69(6):1465–70
- Spinks A, Glasziou PP, Del Mar CB. Antibiotics for sore throat. Cochrane Database of Systematic Reviews 2006, Issue 4. doi:10.1002/14651858.CD000023.pub3
- Sore throat (treatment). ENT UK. www.entuk.org, published 23 January 2012
- Tonsillitis. BMJ Clinical Evidence. www.clinicalevidence.bmj.com, published 26 October 2009
- WHO guidelines on hand hygiene in healthcare. World Health Organization. www.who.int, published 2009









