This information was published by Bupa's Health Content Team and has been reviewed by appropriate medical or clinical professionals. To the best of their knowledge the information is current and based on reputable sources of medical evidence, however Bupa (Asia) Limited makes no representation or warranty as to the completeness or accuracy of the Content.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites.
There are two main types of cervical cancer. Sometimes, cervical cancer can be a mixture of the two types. Squamous cell cancer (the most common) develops in the flat cells covering your cervix. Adenocarcinoma develops in the gland cells that produce mucus, found in the passageway from your cervix to your womb.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites.
There are two main types of cervical cancer. Sometimes, cervical cancer can be a mixture of the two types. Squamous cell cancer (the most common) develops in the flat cells covering your cervix. Adenocarcinoma develops in the gland cells that produce mucus, found in the passageway from your cervix to your womb.
Types of cervical cancer
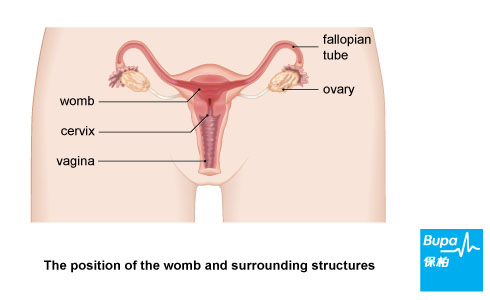
There are two main types of cervical cancer - squamous cell cancer (the most common) and adenocarcinoma, although they are often mixed. They are named after the types of cell that become cancerous. Squamous cells are flat cells covering your cervix; adenomatous cells are found in the passageway from your cervix to your womb. Other rarer cancers of the cervix include small cell cancer.
Symptoms of cervical cancer
If your smear detects abnormal cells on your cervix, they are usually at an early pre-cancer stage, and don't cause any symptoms. Treating the abnormal cells prevents cancer developing.
- abnormal vaginal bleeding, for example between periods or after sex
- smelly vaginal discharge
- pain during sex
- vaginal bleeding after the menopause
- pain in your pelvis
Causes of cervical cancer
The main cause of cervical cancer is the human papilloma virus (HPV). There are over a hundred different types, or strains, of HPV and each type has a specific number. Some types of HPV cause warts and verrucas, and others increase the risk of cervical cancers.
You may have caught this common virus through sex and be unaware that you have it as it usually causes no symptoms. Your immune system may get rid of the infection so you may never be aware of it. Only a very small proportion of women with HPV will develop cervical cancer.
Although HPV is from the same family as the virus that causes genital warts, having genital warts doesn’t make you more likely to develop cervical cancer. Cervical cancer is caused by a different type of HPV.
Risk factors of cervical cancer include:
You may have caught this common virus through sex and be unaware that you have it as it usually causes no symptoms. Your immune system may get rid of the infection so you may never be aware of it. Only a very small proportion of women with HPV will develop cervical cancer.
Although HPV is from the same family as the virus that causes genital warts, having genital warts doesn’t make you more likely to develop cervical cancer. Cervical cancer is caused by a different type of HPV.
Risk factors of cervical cancer include:
- smoking
- having sex at an early age
- having other sexually transmitted infections such as chlamydia and herpes
- having many sexual partners, or have a partner who has had many partners
- taking the contraceptive pill long-term
- having a weakened immune system
Diagnosis of cervical cancer
If you have had an abnormal screening result, or have symptoms of cervical cancer, your doctor will refer you to a gynaecologist (a doctor who specialises in women’s reproductive health).
You may have a number of tests including the following.
You may have a number of tests including the following.
- A colposcopy – your doctor uses a lighted magnifying instrument called a colposcope to examine your cervix and take a small sample of tissue (a biopsy) to be sent to a laboratory for testing to see if the abnormal cells have spread.
- A cone biopsy – your doctor will take a cone of your cervix tissue under general anaesthesia, The sample will be sent to a laboratory for testing.
- LLETZ (large-loop excision of the transformation zone) or loop diathermy – your doctor uses a heated loop of wire to remove the abnormal cells which are then sent to a laboratory for testing.
- A CT, MRI, PET or ultrasound scan – to check your health and show how far the cancer has spread (if at all).
Treatment of cervical cancer
Your treatment will depend on the stage of your cervical cancer and your general health. You may have a combination of treatments. Your surgeon or oncologist will advise you which treatment is best for you.
Surgery
If you have very early stage cervical cancer, a cone biopsy may be all you need.
The most common surgical treatment for cervical cancer is a hysterectomy, including removal of the top few centimetres of your vagina and the lymph nodes in your pelvis.
If you have early stage cancer and still wish to have more children, a radical trachelectomy might be possible. Your surgeon will remove most of your cervix but leave the opening behind, so that you may still have a baby afterwards.
Radiotherapy
Radiotherapy is a treatment to destroy cancer cells with radiation. A beam of radiation is targeted on the cancerous cells, which shrinks the tumour. You may have only radiation, or you may have radiation following surgery.
You may have radiation combined with chemotherapy if the cancer is more advanced or has spread to other areas. This reduces the risk of the cancer coming back. Radiotherapy can be given either from outside the body (external beam radiotherapy) or internally (brachytherapy). These treatments are usually given in sequence.
Chemotherapy
Chemotherapy is a treatment to destroy cancer cells with medicines. It’s used with radiotherapy, or to help to shrink a tumour before radiotherapy or surgery. It can also control symptoms if cancer comes back after an initial treatment.
Surgery
If you have very early stage cervical cancer, a cone biopsy may be all you need.
The most common surgical treatment for cervical cancer is a hysterectomy, including removal of the top few centimetres of your vagina and the lymph nodes in your pelvis.
If you have early stage cancer and still wish to have more children, a radical trachelectomy might be possible. Your surgeon will remove most of your cervix but leave the opening behind, so that you may still have a baby afterwards.
Radiotherapy
Radiotherapy is a treatment to destroy cancer cells with radiation. A beam of radiation is targeted on the cancerous cells, which shrinks the tumour. You may have only radiation, or you may have radiation following surgery.
You may have radiation combined with chemotherapy if the cancer is more advanced or has spread to other areas. This reduces the risk of the cancer coming back. Radiotherapy can be given either from outside the body (external beam radiotherapy) or internally (brachytherapy). These treatments are usually given in sequence.
Chemotherapy
Chemotherapy is a treatment to destroy cancer cells with medicines. It’s used with radiotherapy, or to help to shrink a tumour before radiotherapy or surgery. It can also control symptoms if cancer comes back after an initial treatment.
Prevention of cervical cancer
The following steps may help to reduce your risk of cervical cancer.
- Condoms – using these during sex gives you some protection.
- Regular smears – Department of Health recommends cervical smear screening at 3-yearly intervals for women aged 25-64 after two consecutive normal annual smears have been obtained. Screening may be discontinued in women aged 65 or above if three previous consecutive smears within 10 years are normal. Women who have never had sex or who have total hysterectomy need not receive cervical screening. For women at high risk of developing cervical cancer, for example, immuno-compromised women, annual screening is advised.
- HPV vaccine – HPV vaccine can protect against the HPV strains most likely to cause cervical cancer. There are two HPV vaccines available in Hong Kong. One is Quadrivalent HPV vaccine and another is Bivalent HPV vaccine. The Quadrivalent HPV vaccine indicated in girls and women from the age of 9-45 years and males from the age of 9-15 years, while the Bivalent HPV vaccine indicated in female from the age of 10-25 years.
Common questions
Question: Does human papilloma virus (HPV) cause cancer in men?
Answer: Yes, the human papilloma virus (HPV) is associated with cancer of the penis, anus, and head and neck (tonsils, tongue, and the area at the back of the throat, known as the pharynx).
Explanation: HPV is a common virus that can be passed on through sex but doesn't usually cause symptoms. There are over 100 types of HPV – some of these can cause genital warts and some types are known to increase the risk of developing a particular cancer and are called 'high-risk' HPV. Your immune system usually removes the virus from your body, or the virus can remain in your body without causing any harm for a long time.
High-risk HPV may be a cause of cancer of the penis. It's important to be aware of the symptoms. These include:
Symptoms of head and neck cancer include:
Question: Will treatment for cervical cancer affect my sex life?
Answer: It's usually safe to start having sex again within a few weeks of finishing radiotherapy or having surgery for cervical cancer. However, treatment for cervical cancer may cause an early menopause and radiotherapy can cause side-effects that may affect your sex life.
Explanation: If you haven't yet had your menopause, radiotherapy or surgery to remove your womb and ovaries (hysterectomy) will cause an early menopause. The symptoms are the same as those of a natural menopause. These include:
Radiotherapy may also cause a narrowing of your vagina, a dry vagina, and pain during sex. Talk to your GP about how to manage these symptoms.
You may want to use condoms if you’re having chemotherapy just as a precaution. This is because doctors don’t know whether these medicines can pass to your partner though your vaginal or cervical mucus.
Finally, treatment may make you feel anxious about having sex again and you may not feel like doing so until you have come to terms with your illness.
Question: Will I still need cervical screening tests if I have had the HPV vaccine?
Answer: Yes, if you have had the human papilloma virus (HPV) vaccine you will still need regular cervical screening tests.
Explanation:
There are many different types of HPV. They can be divided into those that are associated with an increased risk of developing certain types of cancer and those that aren't. The HPV vaccine doesn't protect against all types of HPV that are associated with cervical changes and cancer. Therefore, the vaccines don't provide complete protection against the disease. It's thought that the vaccines will prevent at least seven out of 10 of the most common type of cervical cancer (squamous cell cancer).
Therefore, it's important to attend routine cervical screening appointments even if you have had the HPV vaccine.
Answer: Yes, the human papilloma virus (HPV) is associated with cancer of the penis, anus, and head and neck (tonsils, tongue, and the area at the back of the throat, known as the pharynx).
Explanation: HPV is a common virus that can be passed on through sex but doesn't usually cause symptoms. There are over 100 types of HPV – some of these can cause genital warts and some types are known to increase the risk of developing a particular cancer and are called 'high-risk' HPV. Your immune system usually removes the virus from your body, or the virus can remain in your body without causing any harm for a long time.
High-risk HPV may be a cause of cancer of the penis. It's important to be aware of the symptoms. These include:
- a change in the colour, or a thickening, of the skin of your penis
- discharge or bleeding from your penis
- growths or sores, especially under your foreskin
- bleeding from your rectum (back passage)
- pain, discomfort, and itching around your anus
- small lumps around your anus
- faecal incontinence
Symptoms of head and neck cancer include:
- an ulcer that doesn't heal
- difficult or painful swallowing
- pain when you chew
- a constant sore throat
- a lump in your mouth
- numbness in your mouth or lips
Question: Will treatment for cervical cancer affect my sex life?
Answer: It's usually safe to start having sex again within a few weeks of finishing radiotherapy or having surgery for cervical cancer. However, treatment for cervical cancer may cause an early menopause and radiotherapy can cause side-effects that may affect your sex life.
Explanation: If you haven't yet had your menopause, radiotherapy or surgery to remove your womb and ovaries (hysterectomy) will cause an early menopause. The symptoms are the same as those of a natural menopause. These include:
- hot flushes and sweating
- a dry vagina
- low mood
- tiredness
- loss of interest in sex
Radiotherapy may also cause a narrowing of your vagina, a dry vagina, and pain during sex. Talk to your GP about how to manage these symptoms.
You may want to use condoms if you’re having chemotherapy just as a precaution. This is because doctors don’t know whether these medicines can pass to your partner though your vaginal or cervical mucus.
Finally, treatment may make you feel anxious about having sex again and you may not feel like doing so until you have come to terms with your illness.
Question: Will I still need cervical screening tests if I have had the HPV vaccine?
Answer: Yes, if you have had the human papilloma virus (HPV) vaccine you will still need regular cervical screening tests.
Explanation:
There are many different types of HPV. They can be divided into those that are associated with an increased risk of developing certain types of cancer and those that aren't. The HPV vaccine doesn't protect against all types of HPV that are associated with cervical changes and cancer. Therefore, the vaccines don't provide complete protection against the disease. It's thought that the vaccines will prevent at least seven out of 10 of the most common type of cervical cancer (squamous cell cancer).
Therefore, it's important to attend routine cervical screening appointments even if you have had the HPV vaccine.
Resources
Further Information
- Macmillan Cancer Support - 0808 800 0000 - www.macmillan.org.uk
- CancerHelp UK - 0808 800 4040 - www.cancerhelp.org.uk
- Jo's Cervical Cancer Trust - 0808 802 8000 - www.jostrust.org.uk
- Cervical cancer. Cancer Research UK. www.cancerhelp.org.uk, accessed 17 September 2010
- Management of cervical cancer: A national clinical guideline. Scottish Intercollegiate Guidelines Network (SIGN) SIGN 99. 2008. www.sign.ac.uk
- Cervical cancer. Macmillan Cancer Support.www.macmillan.org.uk, accessed 17 September 2010
- HPV and Cervical cancer (in the UK) (WHO/ICC HPV Information Centre). World Health Organization. June 2010. www.who.int
- HPV and cancer. Macmillan Cancer Support. www.macmillan.org.uk, published December 2010









